Experiences of health care workers during the COVID-19 pandemic, September to November 2021
Archived Content
Information identified as archived is provided for reference, research or recordkeeping purposes. It is not subject to the Government of Canada Web Standards and has not been altered or updated since it was archived. Please "contact us" to request a format other than those available.
Released: 2022-06-03
The COVID-19 pandemic has had a significant impact on the health care system, in particular on health care workers on the front lines of caring for Canadians. As the pandemic progressed and cases began to rise, health care workers faced a range of challenges, including extended work hours, decreased vacation time, changes in the methods of delivering care and more. New results from the Survey on Health Care Workers' Experiences During the Pandemic (SHCWEP) show that most health care workers (95.0%) reported that their job was impacted by the pandemic, and a large majority (86.5%) felt more stressed at work during the pandemic.
The SHCWEP was designed to provide insights into the impact of the pandemic on health care workers' mental health, their personal life and their work environment, as well as insights into those who intend to leave their job or change jobs in the coming years and the reasons why they are considering this change. Data from this survey were collected from September to November 2021, coinciding with the fourth wave of the pandemic.
Feeling more stressed at work is the most common impact felt by health care workers during the pandemic
The percentages of all health care workers reporting impacts on their job—for example, changes to the hours they worked, conflict at work or changes to their income—did not differ by gender. While a majority of health care workers in each occupation group reported being impacted by the pandemic, more physicians (96.4%), nurses (96.7%) and other health care workers (for example, dentists, psychologists and medical laboratory technologists) (95.4%) reported being impacted by the pandemic compared with personal support workers (PSWs) or care aides (90.9%).
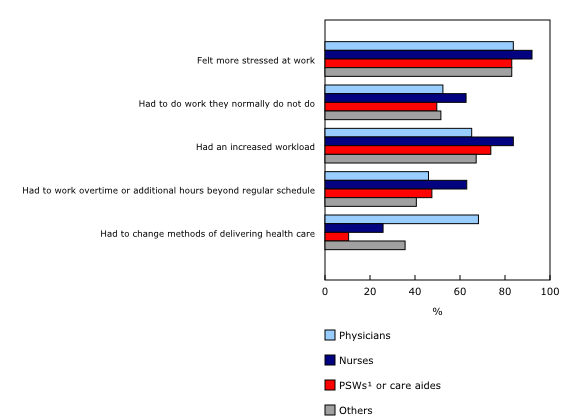
The three job impacts most commonly reported by health care workers were feeling more stressed at work (86.5%), having an increased workload (for example, extra screening, cleaning, and managing personal protective equipment and other tasks related to the pandemic) (74.6%) and having to do work that they do not normally do (55.5%).
Among the occupation groups, about 9 in 10 nurses (92.0%) reported feeling more stressed at work—higher than physicians (83.7%), PSWs or care aides (83.0%) and other health care workers (83.0%). Having an increased workload (83.7%) was the second most commonly reported impact among nurses. Because they often provide hands-on care and work in acute care settings, nurses may not have been able to modify their methods of delivering care and may have had increased demand for their services. Physicians were more likely (68.2%) than people in other occupation groups to report having to change their methods of delivering care, likely reflecting a shift to virtual care.
Nurses are most likely to report intending to change jobs or leave their current job in the next three years, among health care workers not intending to retire
The unprecedented labour demand in the health care system, exacerbated by COVID-19, contributed to the growth in job vacancies in the health care and social assistance sector. Recent results on job vacancies (release of the fourth quarter of 2021) show that there were 126,000 vacancies in the health care and social assistance sector, almost double the number of vacancies seen two years earlier (64,000). The number of job vacancies grew in all health subsectors over the two-year period, led by hospitals (+91.6%; +18,400) and nursing and residential care facilities (+115.0%; +18,800).
Results from the SHCWEP show that among health care workers not intending to retire, 17.9% stated that they intend to leave their current job or change jobs within the next three years, with more women (18.5%) than men (15.5%) considering a change. By occupation group, almost 1 in 4 nurses (24.4%) intended to leave their job or change jobs in the next three years. This result is higher than for other occupation groups: close to 1 in 6 PSWs or care aides (16.4%), over 1 in 8 other health care workers (13.6%) and just over 1 in 10 physicians (11.1%). These differences may reflect the different types of work and job settings within the various occupations. For example, nurses work across a variety of job settings, and the pace and type of work experienced in these settings may differ depending on the patient population nurses are caring for. Nurses working in hospitals or long-term care homes likely would have had to continue to do their work in person, whereas those in outpatient settings may have had the ability to transition to virtual care.
Among those not intending to retire, just over one-fifth of health care workers in acute care (21.1%), congregate living facilities, such as shelters, group homes and prisons (21.0%) (see Note to readers), and long-term care facilities or seniors' residences (20.8%) intended to leave their job or change jobs in the next three years. Health care workers in facilities that provide outpatient and ambulatory care, such as medical and dental offices or clinics, reported the lowest intention to leave their job or change jobs (13.0%). These facilities may have been better able to modify their practices in response to the pandemic—for example, by providing more virtual care or closing completely at times.
A pattern is also noticeable in terms of years of practice. Health care workers with more experience (five years or more) were less likely to intend to leave their job in the next three years than those with less experience. Some of this difference by years of experience may be attributable to the fact that some occupations include rotations or assignments at the beginning of workers' careers, for professional development. Although health care workers may plan to leave their current job or change jobs, they are not necessarily leaving their occupation.
Job stress or burnout is the most common reason why health care workers not intending to retire are considering leaving their job or changing jobs
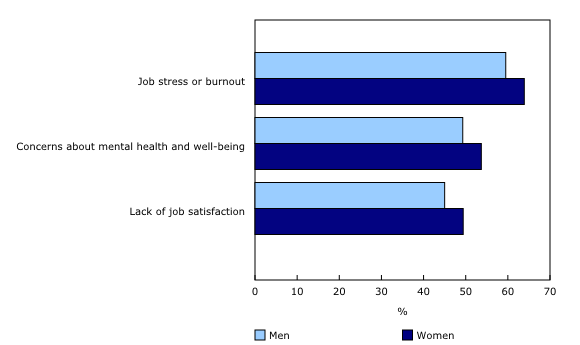
There are differences by gender and occupation type when looking at the reasons health care workers gave for intending to leave their job or change jobs in the next three years. Of those not intending to retire, job stress or burnout was the most commonly reported reason (63.2%) by health care workers. Burnout has been reported by several professional associations as a concern for their members since the onset of the pandemic. The SHCWEP results show that reporting job stress or burnout as a reason for intending to leave their job or change jobs was more prevalent among women (63.9%) than men (59.5%) and among nurses (70.9%) compared with PSWs or care aides (51.0%), physicians (48.2%) and other health care workers (60.6%). The second most common reason why health care workers were considering leaving their job or changing jobs was related to their concerns about their mental health and well-being (53.0%), followed by a lack of job satisfaction (48.8%).
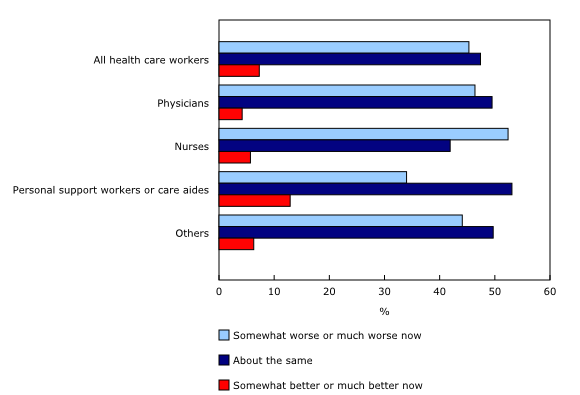
Results from the Survey on Access to Health Care and Pharmaceuticals During the Pandemic show that just over one-third (36%) of the general population surveyed in the spring of 2021 said that their mental health had worsened since the beginning of the pandemic. This rate is even higher in health care workers; according to data from the SHCWEP, 45.3% of health care workers reported that their mental health was "somewhat worse now" or "much worse now" compared with before the pandemic.
The COVID-19 pandemic has highlighted challenges within the Canadian health care system while exacerbating others. The changes observed in the mental health status of health care workers could be temporary and related to unprecedented events. Throughout the pandemic, health care workers have experienced many challenges, such as health risks from exposure to COVID-19 cases, increased workloads, the need to wear personal protective equipment for long periods of time and staffing shortages. Health care workers may continue to be impacted for some time after the pandemic as a result of wait lists and backlogs in health care services because of missed appointments and delayed surgeries and other interventions.
Note to readers
The estimate for congregate living facilities should be interpreted with caution. High sampling variability is associated with the estimate, as the coefficient of variation is greater than 15.0%.
Collection for the Survey on Health Care Workers' Experiences During the Pandemic (SHCWEP) took place between September 2 and November 12, 2021. The survey was developed in collaboration with Health Canada, the Public Health Agency of Canada and the Canadian Institute for Health Information. The 2016 Census was used as the frame, with additional information from the Postsecondary Student Information System. The sample includes health care workers living in the 10 provinces as of May 2016, as well as people following courses of study from 2015 to 2018 that were likely to lead to work in the targeted occupations. Any person working as a health care worker during the pandemic who is not covered by these two groups is considered outside the observed population. There were 24 in-scope National Occupational Classification (NOC) groups for the SHCWEP. Occupations were classified based on the NOC 2016 Version 1.3 using descriptions provided by respondents of the kind of work they were doing and their most important activities or duties. These 24 groups were further combined into four larger occupation groups: physicians (3111, 3112), nurses (3011, 3012, 3233), personal support workers or care aides (3413, 4412), and other health care workers (0311, 3113, 3124, 3131, 3142, 3143, 3211, 3212, 3214, 3222, 3223, 3234, 3411, 4151, 4152, 4153, 4312).
Respondents were asked whether they experienced any of the following impacts on their job during the COVID-19 pandemic: had more conflict among colleagues at work, had more conflict between employees and management, felt more stressed at work, had to do work that they normally did not do, had an increased workload, had to work overtime or additional hours beyond their regular schedule, had reduced hours, were laid off (either permanently or temporarily), had a loss of income, had an increase in income, had to take unpaid leave, were refused vacation or leave, had to change methods of delivering health care, or did not experience any of the above impacts.
Respondents who were currently working as health care workers or in a health care setting were asked how long they were planning to stay in their current job. Categories ranged from less than six months to six years or more. Those who indicated that they were planning to stay in their job for less than three years were asked about the reasons why they might consider leaving their job or changing jobs. Reasons included retirement; job stress or burnout; lack of job satisfaction; concerns about their physical health and safety; concerns about their mental health and well-being; concerns about the physical and mental health of household members or others close to them; financial impacts or concerns; long-term impacts of COVID-19 on the health care system, including changes in methods of delivering health care; another career opportunity; and other. The question did not ask whether the intention to leave their current job or change jobs was related to the COVID-19 pandemic, or whether they were planning to leave their occupation or industry.
For more information on survey definitions and methods, refer to the Statistics Canada survey information page Survey on Health Care Workers' Experiences During the Pandemic.
Contact information
For more information, or to enquire about the concepts, methods or data quality of this release, contact us (toll-free 1-800-263-1136; 514-283-8300; infostats@statcan.gc.ca) or Media Relations (statcan.mediahotline-ligneinfomedias.statcan@statcan.gc.ca).
- Date modified: