Sociodemographic and Socioeconomic Factors Linked to COVID-19 Mortality Rates, 2020-2021
Archived Content
Information identified as archived is provided for reference, research or recordkeeping purposes. It is not subject to the Government of Canada Web Standards and has not been altered or updated since it was archived. Please "contact us" to request a format other than those available.
Released: 2022-03-08
Increasing the use of existing data to explore social and economic factors linked to COVID-19 mortality
In response to the COVID-19 pandemic, Statistics Canada has been releasing provisional death data on a regular basis (Provisional deaths and excess mortality in Canada dashboard). However, on their own, these data have limited ability to explore the social and economic impacts of the pandemic on the Canadian population. Therefore, to expand the value of the provisional death data and create opportunities to explore the social and economic impacts of the pandemic on the Canadian population, Statistics Canada has created a dataset that links the provisional COVID-19 death data from the Canadian Vital Statistics – Death Database with the 2016 Census of Population.
This dataset provides valuable information on the characteristics of Canadians who died of COVID-19 between January 2020 and March 2021. To illustrate the value of this linked dataset, the association of dwelling types, low income status, and the combination of dwelling types and low income status with age-standardized COVID-19 mortality rates were explored. Standardizing the rates by age is important because many of the deaths due to COVID-19 occurred in the senior population.
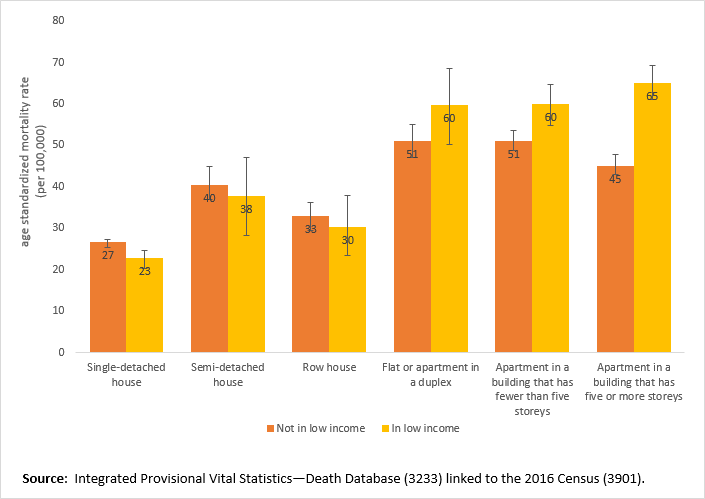
People in low-income households living in high-rise apartments have higher mortality rates due to COVID-19 than those not in low-income households
There were over 10,800 deaths attributed to COVID-19 among Canadians who lived in private homes during the period of January 2020 to March 2021.
Analysis showed that people living in low-income households had significantly higher (1.3 times) COVID-19 mortality rates than people not living in low-income households. This aligns with other analysis using the 2020 Vital Statistics data which showed the mortality rate due to COVID-19 was 1.7 times higher for those in the lowest income neighbourhoods compared with those in the highest income neighbourhoods (13-10-0833-01). The relationship between low income and COVID-19 mortality could be due to low-income households working more in occupations that often require higher contact with the public, such as sales, service and recreation.
The type of dwelling that people lived in was also associated with differences in COVID-19 mortality. People living in detached homes had the lowest mortality rates, while those living in apartments had significantly higher mortality rates. People living in duplexes, low-rise and high-rise apartments had mortality rates around 2 times higher than people living in single-detached houses. Living in multi-residential buildings like apartments could increase the risk of COVID-19 due to the need for frequent close contact with others in high-traffic shared areas like lobbies and elevators.
The combination between the low income status of a household and the type of dwelling showed a unique finding. People who were in a low-income household and lived in an apartment in a multi-storey building had significantly higher COVID-19 mortality rates in comparison to people who lived in other types of dwellings. The COVID-19 mortality rates for people living in a detached house, semi-detached house, row house or duplex did not significantly differ based on low income status. These results suggest that there may be an association between living in a low-income household and COVID-19 mortality for people living in apartments but not for people living in other private dwellings.
There are many factors that can explain this interaction between type of dwelling and low income status on COVID-19 mortality. The increased risk of COVID-19 infection, hospitalization and ultimately mortality is driven by a combination of factors including public contact, geography, income levels, public health restriction compliance, and many others. In its commitment to keeping Canadians informed of the impacts of the pandemic Statistics Canada will continue to explore the sociodemographic and socioeconomic factors associated with COVID-19 mortality in future analyses.
Note to readers
This data analysis is the result of a collaboration between the Public Health Agency of Canada and Statistics Canada.
The probabilistically linked data source used for this analysis included de-identified deaths attributed to COVID-19 that occurred between January 1, 2020 and March 31, 2021 and cause-of-death information from the Provisional Vital Statistics—Death Database linked to the short-form census (2016). There are different ways to measure mortality due to the pandemic. This analysis uses death certificates where COVID-19 is listed as the underlying cause of death. Statistics Canada and provincial and territorial vital statistics agencies use two codes to identify COVID-19 reported as a cause of death: U071 for COVID-19 specified as confirmed by a positive test result, and U072 for COVID-19 described as "possible," "probable," or "pending a (positive) test result."
These results should not be used to estimate overall mortality due to COVID-19 because the analysis is intended to better understand differences in mortality between populations. All the rates presented in this analysis are age-standardized mortality rates, which are used to control for differences in the age structures of the populations being compared. The confidence interval illustrates the degree of variability associated with a rate. Wide confidence intervals indicate high variability, thus, these rates should be interpreted with due caution. When comparing estimates, it is important to use confidence intervals to determine if differences between values are statistically significant.
More information on the linkage process and on the resulting de-identified death-linked analytic file is available upon request (infostats@statcan.gc.ca).
The COVID-19 data in this study are provisional, as they are not based on all deaths that occurred during the reference period because of reporting delays and because they do not include Yukon. A small portion of the deaths attributable to COVID-19 were not linked to the 2016 short-form census and were excluded from this study. Thus, data may not match figures from other sources (e.g., media reports), or from counts and estimates from provincial or territorial health authorities and other agencies. Collective dwellings are not included in these data; as a result, Canadians living in long-term care homes are excluded from the analysis.
Further caution should be used when interpreting the results because sociodemographic and socioeconomic information reported on the Census Day in 2016 may have changed over time. Household characteristics are a portrait of individuals' living arrangements on Census Day. Low income was measured with the adjusted household income compared with the low income measure threshold from the 2016 Census. Refer to the 2016 Census Dictionary for detailed definitions of Census of Population concepts, variables, and geographic terms, as well as historical information.
Contact information
For more information, or to enquire about the concepts, methods or data quality of this release, contact us (toll-free 1-800-263-1136; 514-283-8300; infostats@statcan.gc.ca) or Media Relations (statcan.mediahotline-ligneinfomedias.statcan@statcan.gc.ca).
- Date modified: