Health Reports
The role of neighbourhood environments in hospitalization risk for diabetes and related conditions: A population-based cohort analysis by remoteness and deprivation indices
by Neeru Gupta, Dan Lawson Crouse, Pablo Miah and Tim Takaro
DOI: https://www.doi.org/10.25318/82-003-x202201200001-eng
Abstract
Background
Most socio-epidemiological studies on diabetes incidence, prevalence or hospitalization focus on individual-level risk factors. This population-based cohort study sought to advance understanding on the associations of contextual characteristics and risk of diabetes-related avoidable hospitalization (DRAH) among at-risk Canadians.
Data and methods
A national cohort was compiled from the 2013/2014 Canadian Community Health Survey, representing 5.1 million adults aged 35 years and older reporting having been diagnosed with diabetes, hypertension or heart disease. Their information was linked longitudinally to hospitalization data from the 2013/14 to 2017/18 Discharge Abstract Database as well as to measures of geographic variability from the Material and Social Deprivation Index and the Index of Remoteness. Cox regression models were used to examine associations between the contextual indices and first occurrence of a DRAH.
Results
Residents in the most rural and remote communities were 50% more likely (hazard ratio (HR): 1.51, 95% confidence interval (95% CI): 1.26 to 1.80) to experience a DRAH than those in the most urbanized and accessible communities, and residents in the most socially deprived areas were significantly more likely (HR: 1.44, 95% CI: 1.26 to 1.65) to be hospitalized than those in the most socially privileged areas, controlling for individuals’ sociodemographic characteristics and health behaviours. Neighbourhood material deprivation did not exercise a statistically significant influence on hospitalization risk after adjusting for the other residential characteristics.
Interpretation
There is a clear and significant gradient in diabetes-related hospitalization risk among Canadians with an underlying cardiometabolic condition by degree of residential remoteness and neighbourhood social deprivation, independently of individual characteristics and despite Canada’s universal healthcare system.
Keywords
Diabetes mellitus; social determinants of health; hospitalization; residence characteristics; rural-urban distribution; social deprivation index; data linkage
Authors
Neeru Gupta and Pablo Miah are with the University of New Brunswick, Fredericton, Canada. Dan Lawson Crouse is with the Health Effects Institute, Boston, USA. Tim Takaro is with the Simon Fraser University, Vancouver, Canada.
What is already known on this subject?
- The prevalence of diabetes in adults is increasing in Canada, and there is interest in understanding patient social characteristics that are associated with the risk of diabetes-related hospitalization.
- Previous studies of the social determinants of health and diabetes have focused on individual-level factors, but less is known on how contextual factors may also contribute to inequities in adverse diabetes-related outcomes.
What does this study add?
- This novel study examines the risk of potentially avoidable hospitalization for diabetes and its common comorbidities associated with neighbourhood deprivation and remoteness among Canadian adults with cardiometabolic disease, and this after controlling for individual socio-demographics and health behaviours.
- The study provides good evidence that residents in more socially deprived neighbourhoods and in more rural and remote communities are at greater risk of diabetes-related hospitalization than those residing in more affluent and urbanized areas.
Introduction
The prevalence of diabetes mellitus in adults is increasing in Canada and worldwide because of population aging as well as various social, environmental and genetic factors.Note 1Note 2Note 3 Diabetes is a chronic disease that frequently co-exists with other conditions, and can result in a wide range of acute and long-term complications that may lead to physical and mental limitations, disabilities, and the need for costly hospital services.Note 4Note 5 It has long been suggested, however, that many diabetes-related hospitalizations can be avoided or delayed through appropriate primary and community-based care.Note 6Note 7Note 8Note 9 Given the rising health and economic burden of diabetes to families, communities, workplaces and healthcare systems,Note 10 interest is growing in research on patients’ social characteristics, such as risk and protective factors for hospitalization for diabetes and other ambulatory care sensitive conditions (ACSCs)Note 8Note 11Note 12Note 13Note 14Note 15 that could serve to help inform policy options to reduce health disparities. Until recently, epidemiological studies on diabetes tended to focus on potential individual-level predictors of incidence or prevalence of the disease and its control, but it is increasingly recognized that neighbourhood socioeconomic and physical environmental factors may also contribute to inequities in adverse health outcomes.Note 16 Different features of where people live may influence the distribution of risk factors, such as chronic stressors, food insecurity, tobacco environments, poverty concentration and quality of healthcare.Note 16Note 17Note 18
Research opportunities for assessing the socioenvironmental determinants of diabetes-related avoidable hospitalization (DRAH) are expanding through greater availability of datasets on geographic characteristics linkable to person-level data, notably from administrative hospital inpatient records and household surveys.Note 19Note 20 Some studies have used linked data to examine associations between individual-level and residential characteristics with potentially avoidable hospitalizations among selected urban populations;Note 21Note 22Note 23 other national-level investigations have reported on urban–rural differences as a dichotomous measure.Note 5Note 24 Less well known is how such characteristics influence the risk of DRAHs across the urban‒rural continuum. In other words, few studies explicitly recognize that there is rarely a clear boundary between rural and urban areas, but rather more of a continuum in variation in physical and social community characteristics for the entire population.Note 25Note 26
The objective of this study was to examine different individual and neighbourhood characteristics and their independent associations with risk of hospitalization for diabetes (type 1 or type 2) and selected commonly comorbid conditions among the high-risk Canadian adult population. To adjust for health status in assessing ACSC hospitalizations,Note 7 individuals aged 35 years and older who reported living with diabetes, hypertension or heart disease were included as having a higher risk of DRAHs. The common comorbidities of diabetes included five chronic conditions having management plans with some overlap with the management of diabetes, also known as diabetes-concordant conditions: hypertension, coronary syndrome, heart failure, cardiac arrhythmia and stroke.Note 27Note 28 Using multiple linked datasets, the population-based cohort analysis addressed the question: Do high-risk adults residing in neighbourhoods that are more socially deprived, materially marginalized or more remote have a higher risk of avoidable hospitalization after controlling for individual sociodemographic and behavioural factors? The analysis was further stratified by sex to account for socialized norm differences that may differentially affect the mechanism through which neighbourhood environments affect health outcomes among men and women.Note 17Note 29Note 30Note 31
Data and methods
Study design and target population
This observational cohort study used data on the community-dwelling population from Statistics Canada’s 2013/2014 Canadian Community Health Survey (CCHS) linked to multiple years of hospitalization data from the Discharge Abstract Database (DAD).Note 32Note 33 The baseline cohort was drawn from two years of pooled CCHS cycles, which consisted of information on a range of health-related variables including selected cardiometabolic conditions. The person-level survey response rate was 87.3%.Note 32 The present analysis targeted individuals aged 35 years and older who reported having been diagnosed by a health professional with at least one cardiometabolic condition, which was considered to include diabetes (any type), hypertension (or taken medication for hypertension) or heart disease. Since studies that fail to account for individuals’ health status undermine estimates of the risk of ACSC-related hospitalization,Note 7 respondents who reported not having any of these conditions were excluded.
The second data source used in this study, the DAD, captures standardized administrative, clinical and demographic information on all hospital inpatient stays across Canada (excluding Quebec), collated by fiscal year (i.e., covering the period from April 1 of a given year to March 31 of the next calendar year). Data from CCHS respondents were linked longitudinally to the DAD records of hospital stays using a probabilistic matching approach, which has been detailed methodologically elsewhere.Note 34Note 35Note 36 The present analysis tracked the baseline cohort to their DAD records over five fiscal years, from 2013/14 to 2017/18. While patients may have had multiple hospital records (for one or various conditions), only the first observed diabetes-related admission for each individual was retained. Given differences in reporting of hospital morbidity from Quebec, residents of this province were excluded from the study.
A third kind of data source—geocoded datasets of indices of neighbourhood socioeconomic marginalization and community remoteness—was subsequently used to help examine of the role of areal factors as a social determinant of hospital-based health outcomes. The geographically based data were drawn from the Material and Social Deprivation Index, made available for research use through the Canadian Urban Environmental Health Research Consortium (CANUE),Note 20Note 37 and the new Index of Remoteness, developed by Statistics Canada as a tool for the classification of rurality and remoteness of communities as a relative rather than absolute concept.Note 38Note 39 The person-level cohort data were linked to the census-classified areal data by residential postal code at baseline using the Postal Code Conversion File Plus (PCCF+).Note 40
Hospitalization for diabetes and concordant conditions
The outcome of interest was the risk for an individual to experience a first occurrence of diabetes-related hospital admission over the period of observation (from 2013/14 to 2017/18). Hospital stays as captured in the DAD were flagged based on the primary diagnosis for the length of stay, coded to the standardized International Classification of Diseases, including type 1 and type 2 diabetes (ICD-10-CA codes E10 to E14) and chronic conditions concordant with diabetes: hypertension, coronary syndrome, heart failure, cardiac arrhythmia and stroke (codes I10 to I13, I15, I20, I22 to I25, I50.0, I50.1, I50.9, I48.0, I48.1, and I60 to I64).Note 41
Predictor variables
Contextual hypothesized predictors of DRAH were derived from two open-access datasets. First, the Material and Social Deprivation Index includes two population-based indicators measured at the lowest level of census geography, namely dissemination areas (commonly referred to as neighbourhoods, each targeted to cover about 400 to 700 residents). The quantified dimensions include: (1) a material deprivation index, synthesizing areal measures of the availability of goods and conveniences such as adequate housing, access to high-speed internet and recreational areas; and (2) a social deprivation index, encapsulating fragile social networks such as the proportions of individuals living alone or in single-parent families.Note 37 Both the material and social indices were estimated for the whole of Canada as population percentiles that range from 1 (least deprived neighbourhoods) to 100 (most deprived neighbourhoods). For this study, the 2016 index versions were used, mapped as closely as possible to the cohort’s environmental context for the period of observation. The baseline cohort was ranked into quintile groups against the national percentile distribution (i.e., Quintile 1 as the 20% of adults living with a cardiometabolic condition residing in the country’s least deprived neighbourhoods and Quintile 5 as the 20% of the study population residing in the country’s most deprived neighbourhoods).
Second, the Index of Remoteness dataset gauges the geographic proximity and accessibility of service centres and population centres for all populated census subdivisions (commonly referred to as communities, considered as municipality equivalents).Note 38Note 42 The relative remoteness index ranges in value from 0 (least remote communities, such as those found in the most urbanized parts of southern Ontario, approximating the highest availability and variety of healthcare and other services) to 1 (most rural and remote communities, such as some northern communities lacking year-round connectivity to a main road network). For this study, the baseline cohort was ranked into quintiles of remoteness classes based on the 2016 index values (i.e., Quintile 1 as residents of the 20% most easily accessible communities and Quintile 5 as residents of the 20% most remote communities).
The study further considered several individual-level covariates, as captured in the CCHS, widely attributed in the literature to differential risks of severe cardiometabolic health complications and hospitalization. Specifically, age was measured as a time-varying variable (i.e., from the age at baseline to the age at hospitalization or the end of the study period for those not hospitalized), covering three broad groups across the adult life span: ages 35 to 54 years, ages 55 to 74 years, and ages 75 years and older. Sex (male or female) and marital status (whether or not the respondent is currently in a marital or common-law union) were included as time-invariant demographic variables. Educational attainment (whether or not the respondent attained at least some post-secondary schooling) was considered as a tracer for individual-level socioeconomic status. Also included were two indicators of health-related behaviours: smoking status (whether or not the respondent currently smokes tobacco) and physical activity (whether or not the respondent is active or moderately active in transportation and leisure time based on total daily energy expenditure values).Note 32
Statistical analysis
Following a descriptive data analysis, Cox proportional hazards regression models were used to examine associations between the contextual measures of remoteness and marginalization and the time to the first occurrence of a DRAH, controlling for other individual characteristics as represented below in Equation 1:
(1)
where t represents time and h(t) is the hazard function determined by a set of covariates (x1, x2, x3……xp), with age as a time-varying factor and all other variables as time-invariant measures. The coefficients (b1, b2, b3……bp) measure the impact of the confounders, with h0 as the baseline hazard. The results are expressed in hazard ratios (HRs), that is, exp(bi) in Equation 1, which measures the risk of probability (ranging from 0 to 1) of a diabetes-related hospitalization. Separate models were run for both sexes combined, and then stratified by sex. Only observations with non-missing values for all variables of interest were included in the final analyses.
To account for the CCHS complex sampling design and non-response,Note 32 bootstrap weights were applied to the linked data to ensure population representation and robust 95% confidence intervals (CIs). The sample weights were adjusted by a factor of two to account for the pooling of two years of survey data (i.e., an approach used to increase statistical power).Note 36 The de-identified datasets were accessed in the secure facilities of the New Brunswick Research Data Centre located at the University of New Brunswick. The (unweighted) sample and (weighted) population counts were rounded to meet Statistics Canada data privacy and disclosure protocols using linkable databases.
Results
Determination of the study population
Of the 127,462 individuals aged 12 years and older who responded to the 2013/2014 CCHS,Note 32 101,740 (79.8%) agreed to have their data shared and linked to other datasets (Figure 1). Of these, 27,235 respondents were aged 35 years and older and reported having at least one of the selected cardiometabolic conditions. After excluding from the sample those with missing information on any of the survey-based covariates (1,450 respondents or 5.3%) or contextual indices (1,455 respondents or 5.3%), the final cohort tallied 24,330 survey respondents. Their data were linked to 21,600 hospital records for diabetes and concordant conditions, of which 7,340 were for individuals’ first stays over the quinquennial period from 2013/14 to 2017/18 (the balance of records being readmissions, either at the same or any other hospital, and not considered in the present analyses).

Description for Figure 1
The figure shows a flow chart of the data linkage for the study population.
Of the 127,462 individuals aged 12 years and older who responded to the 2013/2014 CCHS, 101,740 agreed to have their data shared and linked to other datasets. Of these respondents, 20,470 were excluded because they were residents of Quebec and 22,630 were excluded because they were younger than age 35, resulting in a sample of adults aged 35 years and older of 58,650. Of these respondents, 27,235 were aged 35 years and older and reported in the survey having at least one of the selected cardiometabolic conditions. After excluding from the sample 1,450 individuals with missing information on any of the survey-based covariates and 1,455 others with missing contextual indices, the final cohort tallied at 24,330 survey respondents. Their data were linked to 21,600 hospital records for diabetes and concordant conditions, of which 7,340 were for individuals’ first stays over the quinquennial period from 2013/14 to 2017/18. An additional 5,125 Index of Remoteness census subdivisions estimates and 52,734 Material and Social Deprivation Index census dissemination areas estimates were linked to the cohort for analysis.
Source: Linked Canadian Community Health Survey 2013/2014, Discharge Abstract Database 2013/14 to 2017/18, Material and Social Deprivation Index, and Index of Remoteness.
The population-level representation of the final cohort sample reflected 5,138,000 (95% CI: 5,027,000 to 5,249,000) person-years of living with diabetes, hypertension or heart disease. The target population was evenly distributed by sex (Figure 2). One in six (16%) were current smokers, 41% had at most secondary school educational attainment and 53% were physically inactive in their daily lives. In parallel with Canada’s population and service delivery points being heavily concentrated geographically,Note 42 two-thirds (68%) of adults aged 35 years and older living with a cardiometabolic condition resided in one of the 20% most urbanized and accessible areas of the country, while only 2% resided in the most remote areas.

Description for Figure 2
| Category 1 | Category 2 | Category 3 | Category 4 | Category 5 | |
|---|---|---|---|---|---|
| percent | |||||
| Age group | 29 | 53 | 18 | Note ...: not applicable | Note ...: not applicable |
| Sex | 50 | 50 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Marital status | 70 | 30 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Educational attainment | 41 | 59 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Physical activity | 47 | 53 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Tobacco use | 16 | 84 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Relative remoteness | 68 | 18 | 7 | 5 | 2 |
|
Notes: Characteristics drawn from self-reports at baseline. Residential remoteness ranked into quintiles of community accessibility and remoteness, with Quintile 1 = most urban/accessible areas and Quintile 5 = least accessible areas. Data weighted for population representation. Source: Canadian Community Health Survey 2013/2014 (n = 24,330) linked to Index of Remoteness. |
|||||
Descriptive analysis
The rate of first hospitalization for diabetes and related conditions over the five-year observation period averaged 9.9 (95% CI: 9.7 to 10.1) per 100 person-years of living with diabetes, hypertension or heart disease. The proportions of those experiencing a DRAH were higher among those who were older, were male, were not living with a marital partner, had at most a secondary education level, were physically inactive or were tobacco smokers (Figure 3).
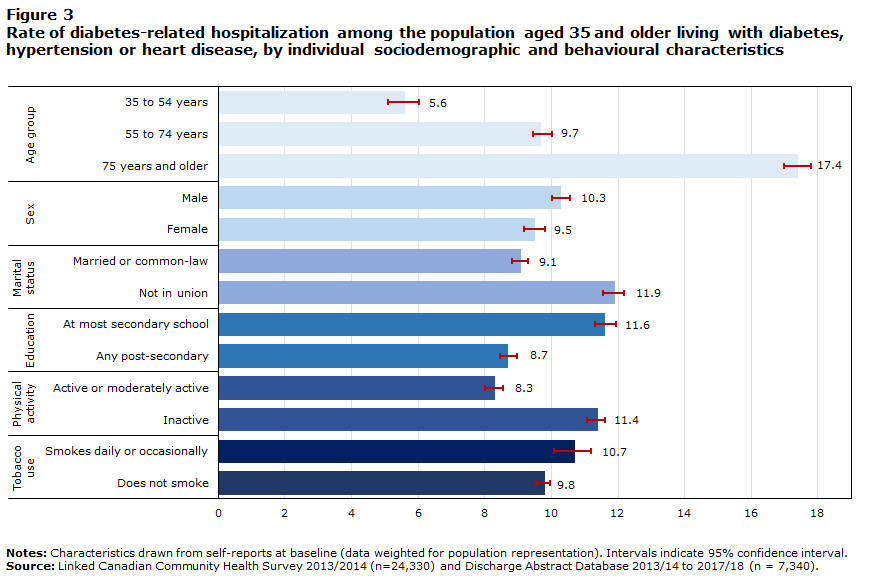
Description for Figure 3
| Per 100 person-years | 95% Confidence interval | ||
|---|---|---|---|
| Lower | Upper | ||
| Age group | |||
| 35 to 54 years | 5.6 | 0.5 | 0.4 |
| 55 to 74 years | 9.7 | 0.3 | 0.3 |
| 75 years and older | 17.4 | 0.4 | 0.4 |
| Sex | |||
| Male | 10.3 | 0.3 | 0.3 |
| Female | 9.5 | 0.3 | 0.3 |
| Marital status | |||
| Married or common-law | 9.1 | 0.3 | 0.2 |
| Not in union | 11.9 | 0.4 | 0.3 |
| Education | |||
| At most secondary school | 11.6 | 0.3 | 0.3 |
| Any post-secondary | 8.7 | 0.3 | 0.3 |
| Physical activity | |||
| Active or moderately active | 8.3 | 0.3 | 0.2 |
| Inactive | 11.4 | 0.3 | 0.2 |
| Tobacco use | |||
| Smokes daily or occasionally | 10.7 | 0.6 | 0.5 |
| Does not smoke | 9.8 | 0.3 | 0.2 |
|
Notes: Characteristics drawn from self-reports at baseline (data weighted for population representation). Intervals indicate 95% confidence interval. Source: Linked Canadian Community Health Survey 2013/2014 (n=24,330) and Discharge Abstract Database 2013/14 to 2017/18 (n = 7,340). |
|||
A direct pattern between the rate of hospitalization and the degree of residential remoteness was observed. The rate increased incrementally by community remoteness quintile, from 9.3 (95% CI: 9.0 to 9.6) per 100 person-years among those residing in the least remote communities to a high of 12.9 (95% CI: 12.3 to 13.7) per 100 person-years in the most remote communities (Figure 4). A similar pattern was seen with regard to the degree of neighbourhood social deprivation; the rate ranged from 8.0 (95% CI: 7.7 to 8.3) per 100 person-years in the least socially deprived neighbourhoods to 12.2 (95% CI: 11.8 to 12.5) per 100 person-years among those residing in the most socially deprived areas. There was less heterogeneity in rates of hospitalization according to quintiles of neighbourhood material deprivation, with 9.6 (95% CI: 9.2 to 9.9) hospitalized per 100 person-years among those residing in the least materially deprived neighbourhoods and 10.5 (95% CI: 10.0 to 10.9) per 100 person-years among those in the most materially deprived neighbourhoods.

Description for Figure 4
| per 100 person-years | 95% Confidence interval | ||
|---|---|---|---|
| Lower | Upper | ||
| Neighbourhood material deprivation | |||
| Quintile 1 | 9.6 | 0.4 | 0.3 |
| Quintile 2 | 9.2 | 0.3 | 0.3 |
| Quintile 3 | 10.4 | 0.3 | 0.4 |
| Quintile 4 | 10.0 | 0.5 | 0.4 |
| Quintile 5 | 10.5 | 0.5 | 0.4 |
| Neighbourhood social deprivation | |||
| Quintile 1 | 8.0 | 0.3 | 0.3 |
| Quintile 2 | 9.6 | 0.3 | 0.3 |
| Quintile 3 | 9.6 | 0.4 | 0.4 |
| Quintile 4 | 10.6 | 0.5 | 0.5 |
| Quintile 5 | 12.2 | 0.4 | 0.3 |
| Community remoteness | |||
| Quintile 1 | 9.3 | 0.3 | 0.3 |
| Quintile 2 | 10.8 | 0.4 | 0.4 |
| Quintile 3 | 11.2 | 0.5 | 0.5 |
| Quintile 4 | 11.7 | 0.4 | 0.4 |
| Quintile 5 | 12.9 | 0.7 | 0.7 |
|
Notes: Baseline cohort ranked into quintiles of residential characteristics, with Quintile 1=least deprived/remote areas and Quintile 5=most deprived/remote areas (data weighted for population representation). Intervals indicate 95% confidence interval. Source: Linked Canadian Community Health Survey 2013/2014, Discharge Abstract Database 2013/14 to 2017/18, Material and Social Deprivation Index, and Index of Remoteness. |
|||
Multivariable analysis for predictors of diabetes-related hospitalization
The results of the Cox regression analysis showed a clear and significant gradient in the risk of hospitalization by quintile of community remoteness, after controlling for other factors. Compared with individuals in the most urbanized communities, residents of communities demarked in Quintile 4 of the Index of Remoteness were 30% more likely to experience a DRAH within five years of baseline (HR: 1.29, 95% CI: 1.14 to 1.46) and those in Quintile 5 were 50% more likely to have been hospitalized (HR: 1.51, 95% CI: 1.26 to 1.80), all else being equal (Table 1). The same significant pattern held when considering each sex separately. For instance, men residing in the most rural and remote communities were significantly more likely to have a DRAH compared with their least rural counterparts (HR: 1.57, 95% CI: 1.21 to 2.05), as were women (HR: 1.40, 95% CI: 1.09 to 1.81).
| Characteristic | Total at-risk population | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| hazard ratio |
95% confidence interval |
p-value | hazard ratio |
95% confidence interval |
p-value | hazard ratio |
95% confidence interval |
p-value | ||||
| from | to | from | to | from | to | |||||||
| Age group | ||||||||||||
| 35 to 54 yearsTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| 55 to 74 years | 1.49Note * | 1.25 | 1.79 | 0.00 | 1.67Note * | 1.33 | 2.10 | 0.00 | 1.28 | 0.96 | 1.71 | 0.09 |
| 75 years and older | 2.42Note * | 2.01 | 2.92 | 0.00 | 2.79Note * | 2.21 | 3.53 | 0.00 | 1.96Note * | 1.47 | 2.61 | 0.00 |
| Sex | ||||||||||||
| MaleTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Female | 0.81Note * | 0.74 | 0.89 | 0.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Marital status | ||||||||||||
| Married or common-law | 0.83Note * | 0.75 | 0.91 | 0.00 | 0.93 | 0.82 | 1.06 | 0.30 | 0.72Note * | 0.63 | 0.84 | 0.00 |
| Not in unionTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Educational attainment | ||||||||||||
| At most secondaryTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Any post-secondary | 0.83Note * | 0.76 | 0.91 | 0.00 | 0.87Note * | 0.76 | 0.98 | 0.02 | 0.78Note * | 0.68 | 0.90 | 0.00 |
| Physical activity | ||||||||||||
| Active or moderately active | 0.74Note * | 0.67 | 0.81 | 0.00 | 0.84Note * | 0.74 | 0.95 | 0.01 | 0.62Note * | 0.54 | 0.71 | 0.00 |
| InactiveTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Tobacco use | ||||||||||||
| Smokes daily or occasionally | 1.12 | 0.99 | 1.26 | 0.08 | 1.10 | 0.94 | 1.30 | 0.24 | 1.16 | 0.96 | 1.39 | 0.12 |
| Does not smokeTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Neighbourhood material deprivation | ||||||||||||
| Quintile 1—least deprivedTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Quintile 2 | 0.95 | 0.83 | 1.09 | 0.49 | 0.97 | 0.81 | 1.17 | 0.78 | 0.92 | 0.77 | 1.11 | 0.40 |
| Quintile 3 | 1.07 | 0.93 | 1.23 | 0.34 | 1.15 | 0.94 | 1.40 | 0.17 | 0.98 | 0.81 | 1.18 | 0.82 |
| Quintile 4 | 0.99 | 0.85 | 1.15 | 0.86 | 0.98 | 0.81 | 1.20 | 0.87 | 0.98 | 0.77 | 1.23 | 0.84 |
| Quintile 5—most deprived | 1.02 | 0.88 | 1.18 | 0.83 | 1.08 | 0.88 | 1.33 | 0.47 | 0.94 | 0.76 | 1.16 | 0.58 |
| Neighbourhood social deprivation | ||||||||||||
| Quintile 1—least deprivedTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Quintile 2 | 1.17Note * | 1.01 | 1.35 | 0.03 | 1.15 | 0.95 | 1.39 | 0.15 | 1.19 | 0.95 | 1.49 | 0.14 |
| Quintile 3 | 1.15 | 1.00 | 1.33 | 0.06 | 1.22 | 1.00 | 1.49 | 0.05 | 1.07 | 0.85 | 1.33 | 0.57 |
| Quintile 4 | 1.27Note * | 1.09 | 1.48 | 0.00 | 1.27Note * | 1.04 | 1.54 | 0.02 | 1.26 | 1.00 | 1.59 | 0.05 |
| Quintile 5—most deprived | 1.44Note * | 1.26 | 1.65 | 0.00 | 1.46Note * | 1.20 | 1.77 | 0.00 | 1.41Note * | 1.16 | 1.71 | 0.00 |
| Community remoteness | ||||||||||||
| Quintile 1—least remoteTable 1 Note † | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable | 1.00 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| Quintile 2 | 1.15Note * | 1.04 | 1.26 | 0.00 | 1.20Note * | 1.05 | 1.36 | 0.01 | 1.10 | 0.96 | 1.26 | 0.18 |
| Quintile 3 | 1.22Note * | 1.08 | 1.38 | 0.00 | 1.23Note * | 1.03 | 1.47 | 0.02 | 1.20Note * | 1.01 | 1.44 | 0.04 |
| Quintile 4 | 1.29Note * | 1.14 | 1.46 | 0.00 | 1.25Note * | 1.03 | 1.51 | 0.02 | 1.35Note * | 1.14 | 1.59 | 0.00 |
| Quintile 5—most remote | 1.51Note * | 1.26 | 1.80 | 0.00 | 1.57Note * | 1.21 | 2.05 | 0.00 | 1.40Note * | 1.09 | 1.81 | 0.01 |
... not applicable
|
||||||||||||
In terms of neighbourhood social deprivation, although the risk gradient was not uniformly statistically evident across the quintiles, residents of the most socially deprived areas were found to be significantly more likely to experience a DRAH than their counterparts in the least socially deprived areas (HR: 1.44, 95% CI: 1.26 to 1.65). The pattern held in the sex-disaggregated models among both men (HR: 1.46, 95% CI: 1.20 to 1.77) and women (HR: 1.41, 95% CI: 1.16 to 1.71).
Neighbourhood material deprivation was not found to exercise a significant influence on hospitalization risk after adjusting for the other residential characteristics. The individual factors of younger age, female sex, being in a marital partnership, higher educational attainment and increased physical activity were each confirmed as independently protective for diabetes-related hospitalizations.
Discussion
This novel cohort study sourced and linked multiple person-level and area-based datasets to examine a parsimonious set of potential correlates of diabetes-related avoidable hospitalization. Among Canadians aged 35 years and older living with a cardiometabolic condition, the rate of being hospitalized at least once for diabetes or a concordant disease averaged 9.9 (95% CI: 9.7 to 10.1) per 100 person-years of exposure. The analysis showed a clear and significant gradient in the risk of DRAHs by degree of community remoteness; residents of the most rural and remote communities were 50% more likely to be hospitalized (HR: 1.51, 95% CI: 1.26 to 1.80) compared with those residing in the most urbanized communities, all else being equal. Such geographic variations, which were also maintained in the sex-disaggregated models, may reflect unequal use of primary care services and other distal determinants of health, such as social isolation and travel burden.Note 43Note 44 Some significant associations between greater neighbourhood social deprivation with risk of DRAH were found, but neighbourhood material deprivation was not found to be independently associated with hospitalization risk. The research thus contributes to the nascent literature on relative remoteness as a meaningful measure of geographic variability in health and healthcare use in Canada’s universal health system.Note 43
At the same time, the individual factors of younger age, female sex, being in a marital partnership, higher educational attainment and being physically active were each found to be independently protective for diabetes-related admissions. Previous studies examining adverse health consequences for age-related diseases limited to traditional markers of socioeconomic status——income, education and occupation—may have been problematic, because they may have different meanings among adults at older ages. The finding that metrics of neighbourhood context were also significantly associated with health outcomes in older adults confirmed that the influence of deprivation persists to the oldest ages.Note 45
The results of this study were, in some ways, consistent with reviews elsewhere supporting a robust link between selected indicators of neighbourhood socioeconomic status with diabetes prevalence, incidence and control.Note 16 However, evidence remains limited on the pathways for how neighbourhood factors contribute to inequalities in hospitalizations, which are among the costliest events to healthcare systems. Few Canadian studies drawing on linked hospital and survey datasets assessing potentially avoidable hospitalizations for ACSCs have been diabetes-specific,Note 14 focused on those most at risk (that is, individuals living with at least one cardiometabolic condition),Note 8 examined jointly the role of both individual- and neighbourhood-level socioeconomic status,Note 15 or investigated geographic variation at the small-area level.Note 46 No studies have assessed the role of relative remoteness and diabetes-related hospitalization among higher-risk Canadians. The current findings provide unique insights into variation in DRAHs by degree of residential rurality, that is, recognizing that rural communities are highly heterogeneous. A small but growing body of research in semi-rural provinces using CANUE datasets is incorporating multiple areal indicators to assess the role of different environmental factors, albeit to mixed results. More research is needed to better understand the interactional effects of individual characteristics and socioenvironmental contexts on protective and risk factors for chronic disease outcomes at the population level in smaller urban and rural settlements.Note 47Note 48
Study strengths and limitations
A key strength of this observational study was the use of multiple kinds of linkable datasets, which allowed for more comprehensive analyses than using survey-, hospital- or areal-based data alone. Because patients hospitalized with diabetes often have other co-existing conditions,Note 49 it was possible to identify those with commonly comorbid cardiometabolic conditions diagnosed in primary care (i.e., information not routinely captured in hospital records). The leveraging of three geographic indices offered indications that the remoteness index may better capture socioenvironmental variations in DRAH than the more extensively used material deprivation index, especially outside of the major urban centres. For ease of interpretation, in the absence of universally accepted cut-off points for geographic classifications,Note 39 the present analysis aggregated the high-risk target population into five equal groups across the ranges of relative areal social deprivation, material deprivation and remoteness. This approach may have yielded a distribution skewness towards areas with higher deprivation and higher remoteness values compared with the general population, as residential socioeconomic marginalization and remoteness have been associated with higher diabetes prevalence, worse rates of diabetes control and greater unmet healthcare needs.Note 16Note 43 Further research is needed on the suitability of other categorizations of geographic indices beyond the five discrete categories that may be related to health and health system outcomes, to complement traditional urban–rural classifications.Note 39
Some limitations to the study are noted. The cohort approach flagged hospital events over the quinquennial period from 2013/14 to 2017/18; however, it should be acknowledged that some individuals may have been hospitalized before the interview, may have received a diagnosis upon hospitalization after the interview at baseline or may have died out of hospital during the follow-up period. Another limitation of the analysis was the static characterization and differences in scale of patients’ residential environments,Note 16 namely that the datasets on areal deprivationNote 37 and remotenessNote 38 were each measured at only one point in time (based on the 2016 census) but also across two levels of geography (neighbourhoods and communities, respectively). Possible effects of bias from missing predictor values or exclusions to the sampling coverage (notably, some First Nations and very remote communities from the CCHS, and facilities in Quebec from the DAD) for assessing hospitalization risk remain unknown. Lastly, the analysis did not consider potential clustering of interactions between individual characteristics and the measured contextual characteristics.Note 16 The study was unable to tease how individuals’ non-financial barriers to accessing and using primary care services (e.g., quality and continuity of care, experiences of discrimination, supportive networks for self-management) may have interacted with indices of service availability in their local communities.Note 7Note 43 Such barriers may be particularly salient for Indigenous populations in Canada who tend to be overrepresented in the remoter areas of the country.Note 43
Conclusion
The results of this study contribute to the increasing body of literature demonstrating that contextual characteristics contribute to, independently from individual-level characteristics, inequities in the risk of potentially avoidable hospitalization of adult Canadians with cardiometabolic conditions. Specifically, this study provides evidence that, after controlling for individuals’ health status, socioeconomic status and health behaviours, residents in more socially deprived neighbourhoods and more rural and remote communities are at greater risk of diabetes-related hospitalization than those residing in more socially privileged and accessible communities.
Acknowledgements
Financial support for this work was received from the Canadian Institutes of Health Research, through the Data Analysis Using Existing Databases and Cohorts operating grant (award number DA4-170257). The data analysis was conducted at the New Brunswick Research Data Centre (NB-RDC), which is part of the Canadian Research Data Centre Network. The services and activities provided by the NB-RDC are made possible by the financial or in-kind support of the Social Sciences and Humanities Research Council, the Canadian Institutes of Health Research, the Canadian Foundation for Innovation, Statistics Canada and the University of New Brunswick. The funders and partners had no role in study design, data analysis and interpretation, preparation of the manuscript, or decision to submit for publication.
- Date modified:
