Insights on Canadian Society
Experiences of Canadians with long-term symptoms following COVID-19
by Sianne Kuang, Steven Earl, Janine Clarke, Dianne Zakaria, Alain Demers, and Samina Aziz
Skip to text
Text begins
Acknowledgments
The Canadian COVID-19 Antibody and Health Survey - Follow-up Questionnaire is the result of a collaboration between the Public Health Agency of Canada and Statistics Canada to understand the long-term impacts of COVID-19 on the lives of Canadians. This study was co-authored by lead analysts from both agencies.
Start of text boxOverview of the study
Using data from the 2023 Canadian COVID-19 Antibody and Health Survey – Follow-up questionnaire (CCAHS-FQ),Note 1 this article provides updated estimates on COVID-19 infections and reinfections among Canadian adults, and describes the nature of symptoms experienced as a result of infection. Results are compared to those from the Canadian COVID-19 Antibody and Health Survey – Cycle 2 (CCAHS-2), which was conducted in 2022, one year before CCAHS-FQ.Note 2 This article also describes the experiences of Canadians who reported long-term symptoms consistent with post COVID-19 condition or long COVID, including the severity of symptoms, their experiences with the health care system, and the impact on their daily lives. Finally, this article also provides updates of the vaccination status of Canadian adults.
- As of June 2023, about two-thirds of Canadian adults reported at least one confirmed or suspected COVID-19 infection, with many reporting more than one infection since the beginning of the pandemic.
- Multiple infections were more commonly reported among certain racialized groups; Black Canadians were most likely to report multiple infections compared to other racialized groups.
- About 3.5 million Canadian adults reported experiencing long-term symptoms following a COVID-19 infection; 2.1 million reported they were still experiencing those symptoms as of June 2023. Almost half of those still experiencing symptoms reported they have not seen any improvement in symptoms over time.
- Among Canadians who were in school or employed and dealing with long-term symptoms, more than 1 in 5 missed days of school or work, missing 24 days on average.
- About 40% of those with long-term symptoms who sought healthcare about their symptoms reported difficulties with access.
- Adults with chronic conditions and senior adults were more likely to have been vaccinated in the 6 months prior to June 2023.
Introduction
Since it was declared an emergency of international concern in January 2020 by the World Health Organization (WHO), COVID-19 has required unprecedented public health action to protect the health of individuals and populations alike.Note 3 In Canada, the pandemic was characterized by waves of infection and subsequent public health measures (including restrictions of in-person activities) with cases becoming more frequent in 2021 and early 2022.Note 4 Initially, the impact of the pandemic was measured by deaths, hospitalizations, and intensive care unit admissions. However, growing population immunity through vaccination and infection, emergence of less virulent variants, and availability of new treatments for acute SARS-CoV-2 infections contributed to the WHO declaring that COVID-19 was no longer an emergency of international concern in May 2023.Note 5
Despite this declaration, COVID-19 continues to cause significant concern for the health of the Canadian population and the wider international community. Accumulating research indicates that COVID-19 is associated with long-term effects on health including the presence of symptoms months or years after the initial infection.Note 6 For some, these long-term symptoms cause significant hardship that affects their health and ability to contribute to society.
To provide initial insights into the burden of long-term symptoms in Canadian adults, the Canadian COVID-19 Antibody and Health Survey Cycle 2 (CCAHS-2) was completed in the summer of 2022. The survey indicated that, as of August 2022, among the approximately 11.8 million Canadian adults that ever had a COVID-19 infection, about 16% experienced long-term symptoms following their infection, and a significant proportion of those affected reported limitations in daily activities and missed time from work or school due to their symptoms.Note 7 These and other results from the CCAHS-2 have helped to improve understanding of COVID-19 infections among Canadians, which is crucial to inform public health policy, economic policy, and respond to the health challenges from COVID-19 as they arise.
To examine the ongoing experiences with and impacts of COVID-19 in Canadian adults more than three years after the start of the pandemic, Statistics Canada, in partnership with the Public Health Agency of Canada (PHAC), conducted a follow-up study (CCAHS-FQ) on the respondents of CCAHS-2 in June 2023.
This study uses data from the CCAHS-FQ to describe the current COVID-19 landscape, including infection, reinfection, and acute and long-term symptoms. This study also uses data from both the CCAHS-2 and the CCAHS-FQ to understand how peoples’ experiences with the virus have evolved in the context of growing immunity, emerging variants, new treatments, and relaxation of public health measures. All results presented from these two surveys relate to the adult population, aged 18 years and older, residing in private households in the 10 Canadian provinces.
In this study, long-term symptoms of a COVID-19 infection refer to the presence of symptoms three or more months after a confirmed or suspected COVID-19 infection that could not be explained by anything else. This definition aligns with the World Health Organization’s post COVID-19 condition case definition, with the exception that the latter requires a symptom duration of at least 2 months. To avoid confusion, this study uses the terminology “long-term symptoms” after COVID-19 infection rather than post COVID-19 condition.
Start of text boxWorld Health Organization definition of Post COVID-19 Condition
Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others which generally have an impact on everyday functioning. Symptoms may be new onset, following initial recovery from an acute COVID-19 episode, or persist from the initial illness. Symptoms may also fluctuate or relapse over time.Note 7
As of June 2023, about 2 in 3 Canadians reported at least one infection with 1 in 5 having been infected multiple times
It is expected that the number of COVID-19 reinfections will grow as the percentage of the population ever having COVID-19 grows, antibody levels decline over time, and novel variants with increased ability to evade immunity emerge. The percentage of Canadian adults who tested positive for COVID-19 or suspected a COVID-19 infection since the start of the pandemic increased from 38.7% in the summer of 2022 as reported in CCAHS-2 to 64.4% by June 2023 as reported in the CCAHS-FQ. At this point, 44.6% of Canadians had experienced one, 14.4% two, and 5.4% three or more infections. While cases surged in the early months of 2022, infections have continued through to June 2023. In fact, in the three months prior, 8.9% of Canadian adults reported being infected. In the six months prior, the proportion was 13.7%.
These numbers likely underestimate the true number of infections by June 2023, as individuals are not always aware that they have been infected. Results from CCAHS-2 showed that during the summer of 2022, 41.2% of Canadians with antibodies from a past infection never previously tested positive nor suspected an infection.Note 8
Infection and reinfection varied by age. As displayed in Chart 1, older adults were less likely to report multiple infections. This could be attributed to the increased risk of severe disease from COVID-19 for older adults leading this group to take more precautions against a COVID-19 infection.Note 9 Males more frequently reported not having had a previous COVID-19 infection than females, but both males and females were similarly likely to report multiple COVID-19 infections. Reinfection reporting also differed across racialized groups. Black (30.3%) Canadians more frequently reported having multiple infections than Canadians with Latin American (21.7%), Chinese (18.3%), Filipino (17.9%), Arab (12.1%) and West Asian (9.1%) backgrounds. Previous studies have shown that some populations in Canada were more adversely impacted by the pandemic. For example, in 2020, Black and South Asian populations were found to have a much higher mortality rate due to COVID-19 than non-racialized and non-Indigenous groups.Note 10

Data table for Chart 1
| Age group | 3 or more infections | 95% confidence intervals | 2 infections | 95% confidence intervals | 1 infection | 95% confidence intervals | 0 infections | 95% confidence intervals | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| lower bound | upper bound | lower bound | upper bound | lower bound | upper bound | lower bound | upper bound | |||||
| percent | ||||||||||||
| 18 to 34 years | 6.7 | 5.0 | 9.1 | 18.0 | 14.8 | 21.7 | 46.4 | 42.0 | 50.9 | 28.8 | 24.9 | 33.2 |
| 35 to 49 years | 8.2 | 6.2 | 10.8 | 19.6 | 16.9 | 22.7 | 46.0 | 42.3 | 49.7 | 26.2 | 23.0 | 29.7 |
| 50 to 64 years | 4.0 | 3.0 | 5.4 | 12.2 | 10.3 | 14.3 | 45.9 | 42.8 | 49.1 | 37.9 | 34.7 | 41.2 |
| 65 years and over | 2.3Note E: Use with caution | 1.6 | 3.3 | 6.9 | 5.6 | 8.5 | 39.6 | 36.8 | 42.4 | 51.2 | 48.2 | 54.2 |
|
E use with caution Note: Some estimates do not add correctly due to rounding. Source: Statistics Canada, Canadian COVID-19 Antibody and Health Survey - Follow-up Questionnaire, 2023. |
||||||||||||
People have experienced symptoms differently since the emergence of Omicron compared to before
Throughout the pandemic, fatigue, fever, coughing, and sore throat have remained the most commonly reported acute symptoms, however some symptoms have become more common since the emergence of Omicron in December 2021. Most notably, the percentage reporting cough rose from 41.7% to 55.2%, nasal congestion from 30.2% to 42.4%, and sore throat from 41.6% to 52.8%. Other studies have found minor variation in symptoms across variants.Note 11
In January 2022, prescription medications were approved for the treatment of COVID-19 infections.Note 12 Among Canadian adults reporting a COVID-19 infection since then, 3.1% reported taking such medication. Of these, 77.1% reported the medication was effective or very effective. Use of prescription medication increased with age and was more common among those with a pre-existing long-term health condition. Both are populations at higher risk of more severe disease or outcomes from a COVID-19 infection.Note 13 This result aligns with Health Canada’s authorization of the use of prescription anti-viral medication for patients at high risk of developing serious disease.Note 12
1 in 9 Canadian adults have experienced long-term COVID-19 symptoms; most continue to experience symptoms
The increased rate at which long-term symptoms occur in those with COVID-19 infections is an observed phenomenon that sets the illness apart from other respiratory viruses, such as the flu.Note 14 This may be related to the fact that COVID-19 affects a wide range of body systems, not limited to the respiratory system, and has been documented to be able to cause organ damage in infected individuals.Note 15
As of June 2023, 19% of Canadian adults infected reported ever experiencing long-term symptoms (symptoms present 3 or more months after a COVID-19 infection). This represents 11.7% of the total adult population or 3.5 million Canadians living in the ten provinces. The current burden, measured in June 2023, is also substantial: 6.8% of all Canadian adults or 2.1 million people continue to experience long-term symptoms. On average, this group had their most recent COVID-19 infection 11 months prior.
Some Canadians were at greater risk of experiencing long-term symptoms following a COVID-19 infection. Adults with a self-reported disability were more likely to report long-term symptoms than those without a reported disability (26.8% vs. 18.3%), and adults reporting one or more chronic conditions prior to the start of the pandemic were more likely to report long-term symptoms than adults not reporting chronic conditions (24.7% vs. 14.0%). Other studies have demonstrated an association between pre-existing medical conditions and the development of long-term symptoms.Note 16
Despite many different long-term symptoms having been reported, some occurred more often than others, with fatigue (65.5%), brain fog (39.0%) and shortness of breath (28.0%) being the most frequently reported. These long-term symptoms have also been reported in other international contexts.Note 17 Differences are observed in the frequency of some long-term symptoms before and after the emergence of Omicron. For example, since the emergence of Omicron, individuals with long-term symptoms were more likely to report feeling worse after physical or mental activity, coughing and fatigue, and less likely to report loss of smell or taste and headache.
Long-term symptoms may take longer than three months to develop or return after an initial recovery. Among individuals who reported not experiencing symptoms three months or longer after a COVID-19 infection in the summer of 2022, 11.1% have since reported developing long-term symptoms after that same infection that could not be explained by anything else.
Start of text boxThe percentage of adults experiencing long-term symptoms increased with the number of COVID-19 infections reported
The potential impact of re-infections on the risk of developing or exacerbating pre-existing long-term symptoms is important considering the endemic nature of COVID-19. However, studies providing evidence of increased risk are limited in number and generalizability.Note 18 As seen in Chart 2, Canadians reporting two known or suspected COVID-19 infections (25.4%) were 1.7 times more likely to report prolonged symptoms than those reporting only one known or suspected infection (14.6%), and those with 3 or more infections (37.9%) 2.6 times more likely.
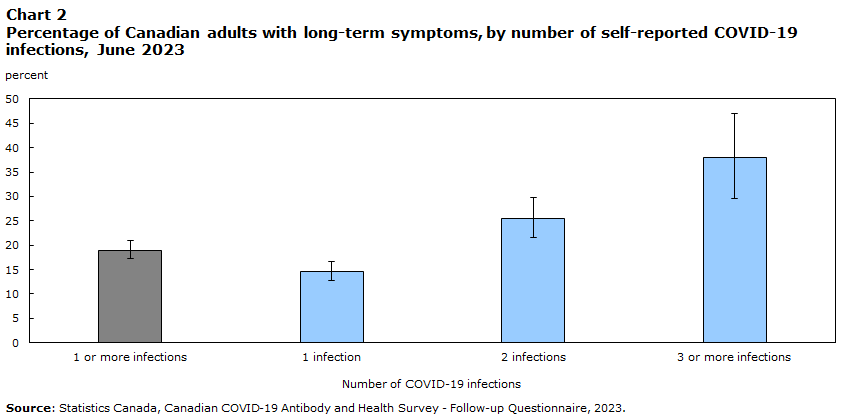
Data table for Chart 2
| Number of COVID-19 infections | People with long-term symptoms | 95% confidence intervals | |
|---|---|---|---|
| lower bound | upper bound | ||
| percentage | |||
| 1 or more infections | 19.0 | 17.3 | 20.9 |
| 1 infection | 14.6 | 12.8 | 16.7 |
| 2 infections | 25.4 | 21.5 | 29.7 |
| 3 or more infections | 37.9 | 29.5 | 47.0 |
| Source: Statistics Canada, Canadian COVID-19 Antibody and Health Survey - Follow-up Questionnaire, 2023. | |||
People that had their first infection early in the pandemic, though, were also more likely to report multiple COVID-19 infections. For example, in this study the average date of first infection for those with three or more infections was May 2021, compared to September 2021 for those with two infections, and May 2022 for those with one infection. Those infected earlier in the pandemic, before vaccination and the emergence of the Omicron variant were more likely to develop long-term symptoms, but also had more time since their first infection to become infected with COVID-19 again.Note 19 This may help to explain the relationship between number of COVID-19 infections and the development of long-term symptoms. However, as displayed in Table 1 below, a positive association is observed throughout time when examining the above relationship by period of first COVID-19 infection, suggesting that time period of first infection may not fully account for this correlation. In addition, since the follow-up questionnaire did not capture the exact sequencing of infections and long-term symptoms, it is also possible that certain immune responses in people that develop long-term symptoms may increase susceptibility to re-infection.Note 15
| Period of first infection | Number of COVID-19 infections | People ever reporting long-term symptoms | 95% confidence intervals | |
|---|---|---|---|---|
| lower bound | upper bound | |||
| percentage | ||||
| January 2020 to December 2020 | 1 | 14.2Note E: use data with caution | 9.0 | 21.7 |
| 2 | 34.1 | 25.9 | 43.3 | |
| 3 or more | 45.3Note E: use data with caution | 31.0 | 60.4 | |
| January 2021 to December 2021 | 1 | 17.8Note E: use data with caution | 12.0 | 25.5 |
| 2 | 18.8 | 13.5 | 25.7 | |
| 3 or more | 31.1Note E: use data with caution | 16.8 | 50.1 | |
| January 2022 to December 2022 | 1 | 13.3 | 11.4 | 15.5 |
| 2 | 25.8 | 19.8 | 32.8 | |
| 3 or more | 33.9Note E: use data with caution | 23.3 | 46.4 | |
|
E use data with caution Source: Statistics Canada, Canadian COVID-19 Antibody and Health Survey - Follow-up Questionnaire, 2023. |
||||
Almost half of Canadians who reported that they continue to experience long-term symptoms also reported no improvement over time
Many Canadians with long-term symptoms experience a protracted symptom duration. As of June 2023, 58.2% of infected Canadians who ever reported long-term symptoms continue to experience them. Among Canadian adults who continued to experience long-term symptoms, 79.3% had been experiencing symptoms for 6 months or more, including 42.2% with symptoms for one year or more (Figure 1).
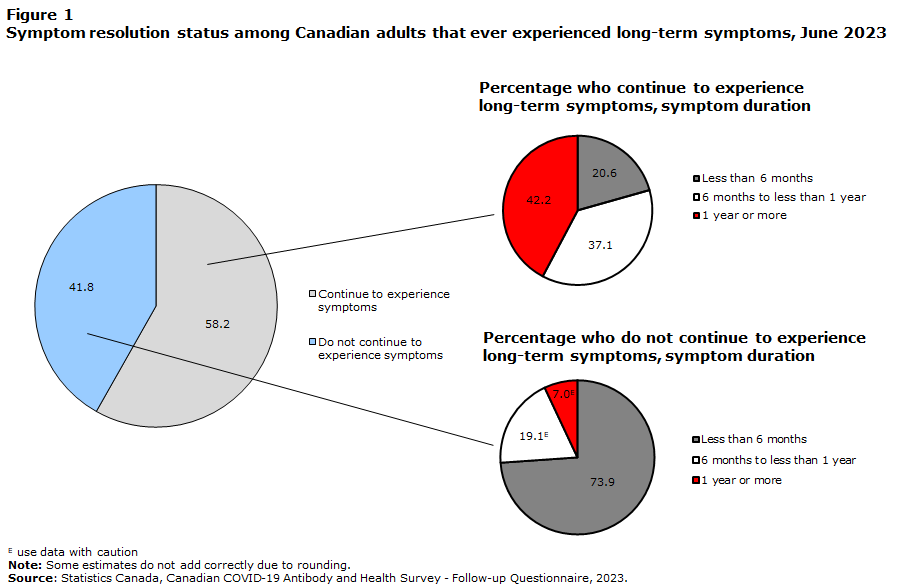
Data table for Figure 1
| Symptom resolution status | Symptom duration | ||||
|---|---|---|---|---|---|
| Continue to experience symptoms | Do not continue to experience symptoms | Less than 6 months | 6 months to less than 1 year | 1 year or more | |
| percentage | |||||
| People ever reporting long-term symptoms | 58.2 | 41.8 | Note ...: not applicable | Note ...: not applicable | Note ...: not applicable |
| People still experiencing long-term symptoms | Note ...: not applicable | Note ...: not applicable | 20.6 | 37.1 | 42.2 |
| People no longer experiencing long-term symptoms | Note ...: not applicable | Note ...: not applicable | 73.9 | 19.1Note E: Use with caution | 7.0Note E: Use with caution |
|
... not applicable E use with caution Note: Some estimates do not add correctly due to rounding. Source: Statistics Canada, Canadian COVID-19 Antibody and Health Survey - Follow-up Questionnaire, 2023. |
|||||
Start of text box
Of those who reported experiencing long-term symptoms in the CCAHS-2 in the summer of 2022, 72.5% continued to experience symptoms one year later.
Depending on the nature, severity and frequency of long-term COVID-19 symptoms, the effects of such symptoms on an individual can range from mild to debilitating. Among Canadians who continue to experience symptoms, about 70% reported experiencing them every day or almost every day when symptoms were at their worst, and 21.7% reported being often or always limited by them in their daily activities. Overall, 49.7% with ongoing symptoms reported no improvement in their symptoms over time. Among Canadians who reported ever experiencing long-term symptoms, females (33.0%) were less likely than males (53.1%) to report a resolution of their symptoms and experienced their symptoms longer on average (see Chart 3).
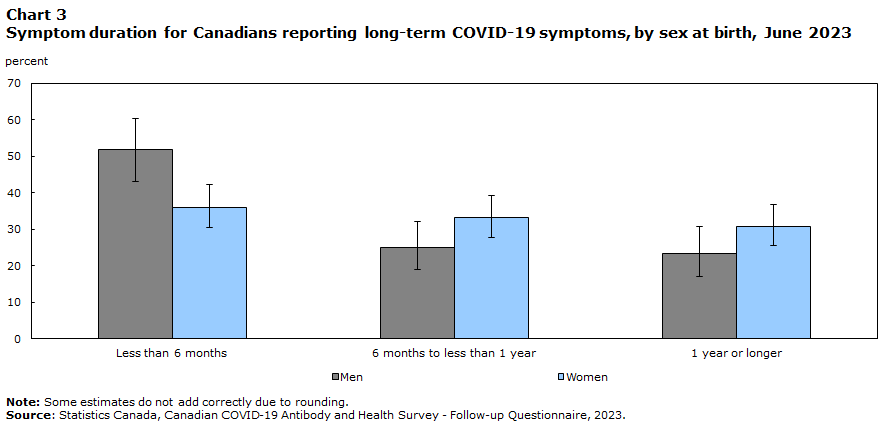
Data table for Chart 3
| Long-term symptom duration | Men | 95% confidence intervals | Women | 95% confidence intervals | ||
|---|---|---|---|---|---|---|
| lower bound | upper bound | lower bound | upper bound | |||
| percentage | ||||||
| Less than 6 months | 51.8 | 43.1 | 60.3 | 36.0 | 30.3 | 42.1 |
| 6 months to less than 1 year | 25.0 | 19.0 | 32.1 | 33.2 | 27.7 | 39.3 |
| 1 year or longer | 23.3 | 17.1 | 30.8 | 30.8 | 25.6 | 36.6 |
|
Note: Some estimates do not add correctly due to rounding. Source: Statistics Canada, Canadian COVID-19 Antibody and Health Survey - Follow-up Questionnaire, 2023. |
||||||
As of June 2023, more than 1 in 5 Canadians with long-term symptoms missed days of work or school
Results of the CCAHS-FQ show that long-term symptoms interfere with many Canadians’ livelihoods and education. Among Canadian adults ever experiencing long-term symptoms who were employed or attending school, 22.3% missed days. On average, they missed 24 days of school or work. This translates to 600,000 Canadians missing time from work or school and a cumulative total of about 14.5 million missed days of work or school due to long-term symptoms.
Among employed Canadian adults reporting ever experiencing long-term symptoms, 5.3% applied for disability benefits or workers’ compensation due to their symptoms, and 93.8% of those who applied received benefits or compensation. Among those working Canadians reporting long-term symptoms, the most common industries they worked in were healthcare and social assistance (17.5%), professional, scientific and technical services (17.1%), and educational services (10.3%). As of June 2023, about 100,000 Canadian adults have been unable to return to work or school because of their symptoms.
Some estimates of the impact of long-term symptoms on work and school may differ from those previously reported because this study focuses on impacts experienced three or more months after a COVID-19 infection.
Only 1 in 8 Canadians who sought help for their long-term symptoms felt they received adequate care
While many Canadians have needed healthcare because of COVID-19 in the past few years, the pandemic complicated many Canadians’ access to these services. Factors, including restricted entry into healthcare facilities due to public health protocols and the absence of medical personnel due to illness, slowed the delivery of healthcare services. While virtual care was expanded to service Canadians during the pandemic, these services are not always appropriate depending on clinical needs.Note 20
As of June 2023, 46.9% of Canadian adults with long-term symptoms consulted with a healthcare provider or service about their symptoms. Family doctors and nurse practitioners continue to be the main point of contact for most Canadians for their healthcare needs, as 82.8% of the above group reported consulting with either of these professionals about their long-term symptoms. Studies from other countries have found a similar percentage of people with post COVID-19 condition consulted a general practitioner about their condition.Note 21 The other most frequently reported healthcare services consulted for long-term symptoms were specialist medical doctors (20.0%), pharmacists (18.7%), and emergency departments (17.0%). Of those who accessed a healthcare service for their long-term symptoms, the average number of different services consulted was two.
According to the CCAHS-FQ, 39.7% of those who consulted a healthcare provider or service about their long-term symptoms also reported at least one difficulty accessing those providers or services. Of the 800,000 Canadians with long-term symptoms who reported difficulty accessing a healthcare provider or service, 1 in 5 did not receive that service because of their reported difficulties. Among those who reported difficulties, the most frequently reported problems accessing healthcare were: waiting too long between booking an appointment and a healthcare service (49.4%), having an appointment cancelled, rescheduled, or delayed due to the pandemic (39.6%), and difficulty getting a referral (35.2%).
Being able to consult with a healthcare professional does not necessarily ensure that an individual’s need for treatment was fully met. In fact, 66.4% of those with long-term symptoms who needed healthcare services felt they did not receive adequate treatment, service, or support for any of their symptoms. Only 12.5% of Canadian adults who needed healthcare for their long-term symptoms reported receiving treatment, services, or support for all their symptoms, and among those who continue to experience long-term symptoms as of June 2023, only 5.7% received a post COVID-19 condition diagnosis.
Start of text boxOlder adults are more likely to keep up to date with their vaccinations against COVID-19
COVID-19 vaccines reduce the risk of severe disease, hospitalization, and death.Note 22 Some research also suggests that vaccination may also lower the risk of developing long-term symptoms.Note 23 Results from the CCAHS-FQ indicate that as of June 2023, 93.0% of Canadian adults had received one or more COVID-19 vaccine doses: less than 1 percent had received one, 13.8% two, 29.4% three, and 49.2% four or more. With respect to recency of last vaccine dose, 18.3% of the Canadian adult population were last vaccinated in the 6 months prior to the CCAHS-FQ, but this varied by age group and number of chronic conditions present prior to the start of the COVID-19 pandemic.
Staying up to date with COVID-19 vaccinations is particularly important for people at high risk of adverse outcomes, including people aged 65 years and older, and people with pre-existing long-term health conditions.Note 24 Adults 65 years and older (34.5%) were more likely to have received a vaccination in the six months prior to June 2023, compared to 50 to 64 year olds (18.1%), and 18 to 49 year olds (10.5%). Adults with three or more pre-existing chronic conditions (28.4%) were more likely to have received a vaccination in the six months prior to survey collection compared to adults with two chronic conditions (23.9%), 1 chronic condition (20.4%), and no chronic conditions (14.1%). Flu vaccine uptake trends also show a higher coverage rate for adults aged 65 years and older.Note 25
Conclusion
Using data from the CCAHS-FQ and the CCAHS-2, this study depicts how COVID-19 has evolved in the Canadian landscape more than three years into the pandemic. The results show that 1 in 5 Canadian adults have experienced COVID-19 more than once, and that many Canadians currently experience long-term symptoms from a COVID-19 infection. For the latter group, these symptoms often have strong implications on many facets of their lives, including their ability to perform daily activities, work and go to school. The study adds to a growing body of evidence around the association between COVID-19 reinfection and the reporting of long-term symptoms.
Among Canadians who reported ever experiencing long-term symptoms, those who continue to experience these symptoms (58.2%) outnumber those who have reported them resolved (41.8%). As of June 2023, an estimated 2.1 million Canadian adults continued to experience long-term symptoms after a confirmed or suspected COVID-19 infection that could not be explained by anything else. Almost 80% of these adults had been experiencing long-term symptoms for 6 or more months and about half reported no improvement in their symptoms over time. When at their worst, these symptoms often or always limited daily activities for more than 1 in 5 Canadian adults who continued to experience long-term symptoms at the time of the survey. In addition, among adults who experienced long-term symptoms and were employed or attending school, more than 1 in 5 missed days because of their symptoms.
With about 2 in 5 affected Canadian adults accessing healthcare for their long-term symptoms, awareness of the condition and evidence-based methods for diagnosing, treating, and managing it are important. However, this study found that a substantial number of adults with long-term symptoms experienced difficulties accessing healthcare for their symptoms, and 2 in 3 who needed healthcare services reported not receiving treatment, services or support for any of their symptoms. Considering these findings, protection against COVID-19 infections including reinfections and the development of long-term symptoms is paramount. While 93% of Canadian adults have received at least one COVID-19 vaccine dose, only 18.3% received their most recent dose in the 6 months prior to June 2023.
Sianne Kuang, Steven Earl, and Janine Clarke are analysts with the Centre for Direct Health Measures at Statistics Canada. Dianne Zakaria, Alain Demers, and Samina Aziz are analysts with the Public Health Agency of Canada.
Start of text box
Data sources, methods, and definitions
Data sources
Data are primarily from the Canadian COVID-19 Antibody and Health Survey – Follow-up Questionnaire (CCAHS-FQ) administered by Statistics Canada in collaboration with the Public Health Agency of Canada. Respondents included adults aged 18 and older living in the 10 provinces who had previously participated in the Canadian COVID-19 Antibody and Health Survey – Cycle 2 (CCAHS-2). Excluded from the survey were: persons living in the three territories; persons living on reserves and other Indigenous settlements in the provinces; members of the Canadian Forces living on a base; the institutionalized population; and residents of certain remote regions. All estimates in the study should be assumed to be from the follow-up survey unless an external source is explicitly stated, or the reference year of the estimate is 2022. In the latter case, the source of the estimate is the CCAHS-2. Data on long-term health conditions are sourced from CCAHS-2, only long-term health conditions diagnosed by a healthcare professional were included. A list of the conditions can be found in the questionnaire.
CCAHS-FQ
The CCAHS-FQ was conducted between May and June 2023. The survey collected information on vaccination status, reinfection with the virus that causes COVID-19, and symptoms of COVID-19, including long-term symptoms and their impact on daily life, health conditions and the use of health care services.
Survey weights were used to create a representative sample and to minimize any potential bias that could arise from the follow-up survey non-response. Non-response adjustments and calibration using available auxiliary information were also applied and are reflected in the survey weights.
CCAHS-2
The CCAHS-2 was conducted between April and August 2022. The CCAHS-2 survey consisted of two parts. The first part was an electronic questionnaire about general health and experiences with COVID-19, including long-term symptoms. The second part included two self-administered sample collections: an at-home finger-prick sample collection called a dried blood spot (DBS) sample and a saliva sample. The DBS was used to measure the presence of antibodies against SARS-CoV-2, the virus that causes COVID-19, from vaccination or prior infection. The saliva sample was used to determine if there was a recent or current SARS-CoV-2 infection at the time of sampling, by testing for viral material in the sample using a polymerase chain reaction (PCR) test.
Definitions
Confirmed or suspected COVID-19 infection
A confirmed infection refers to an infection that is determined by a positive COVID-19 test result, whether it is a PCR test or an at-home rapid antigen test. A suspected infection is based on the presence of symptoms or recent contact with a COVID-19 infected person.
Long-term symptoms
Long-term symptoms of a COVID-19 infection refer to the presence of symptoms three or more months after confirmed or suspected COVID-19 infection that could not be explained by anything else.
Long-term health conditions or chronic conditions
In the initial survey (CCAHS-2), respondents were asked a series of questions about long-term health conditions. These are conditions which are expected to last or have already lasted 6 months or more and have been diagnosed by a health professional.
Strengths and limitations
The main strength of the present analysis is that it is based on a nationally representative survey of Canadian adults. The large sample allowed a wide variety of analyses to be conducted in order to best describe the current COVID-19 situation in Canada.
A limitation of the present study is that it relies on self-reported information about infections and experiences since the beginning of the pandemic, which some people may not be able to remember accurately, especially as time goes on. It is also subject to recall bias, where a person’s current state may influence their recollection of the past. Further, with regards to past infections, respondents were asked to include both confirmed and suspectedCOVID-19 infections; it is possible that a person reported one or more suspected COVID-19 infections that were due to a different virus. Data from CCAHS-2, which tested for the presence of COVID-19 antibodies, showed that some people who reported a suspected infection in 2022 did not have detectable antibodies due to an infection. By contrast, there were also people in CCAHS-2 who tested positive for antibodies from a past infection but did not report a past infection (were unaware). In addition, distinguishing between different infections and long-term symptoms may have been difficult. Some reported new infections could have been related to a persistent past infection or the development of long-term symptoms. Conversely, it is possible that some people were experiencing symptoms from a new infection, rather than long-term symptoms from a past infection. Finally, although there was a large sample that responded to the CCAHS-FQ, it was only about one-third of those who had responded to the CCAHS-2, being limited, in part, by the availability of valid email addresses for follow-up. While the survey weights were adjusted to account for non-response and incomplete coverage, it is possible that those who had more infections or had more symptoms, etc. were more likely to respond to the CCAHS-FQ.
- Date modified:
