 StatCan COVID-19: Data to Insights for a Better Canada COVID-19 death comorbidities in Canada
StatCan COVID-19: Data to Insights for a Better Canada COVID-19 death comorbidities in Canada
Archived Content
Information identified as archived is provided for reference, research or recordkeeping purposes. It is not subject to the Government of Canada Web Standards and has not been altered or updated since it was archived. Please "contact us" to request a format other than those available.
by Kathy O'Brien, Marylène St-Jean, Patricia Wood, Stephanie Willbond, Owen Phillips, Duncan Currie and Martin Turcotte
Text begins
There is now clear evidence that people with pre-existing chronic conditions or compromised immune systems are at higher risk of dying of COVID-19Note , especially among those over the age of 80. It is now possible, using provisional results from the Canadian Vital Statistics Death Database (CVSD), to identify the most common chronic conditions among Canadians who have died from COVID-19 during the first wave of the pandemic.
In Canada, the Canadian Vital Statistics Death Database (CVSD) is the authoritative source for cause of death data, including COVID-19 deaths. In addition to identifying the underlying cause of death, the CVSD also includes information on the contributing causes and conditions (or comorbidities). In the context of a death caused by COVID-19, these include other diseases or conditions, such as diabetes or hypertension, that likely put those individuals at higher risk of death from COVID-19. While there may be challenges associated with the distinction between chronic conditions and other causes, as well as the nature of these with respect to COVID-19, the CVSD data provides additional insight on COVID-19 related deaths.
Using the latest multiple cause of death data from the CVSD, this article presents information about the most common chronic and acute conditions, diseases, disorders, and complications appearing on the medical certificate of cause of death where COVID-19 was involved in the death, to provide preliminary insights to COVID-19 comorbidities. This does not consider the relative importance of the additional disease or condition, nor its relationship to COVID-19, and is similar to that used by the by the National Center for Health Statistics in its weekly COVID-19 updates.Note Also examined is the extent to which these diseases and conditions differ by sex and by age groups.
Unless otherwise stated, the data in this paper are based on deaths in the CVSD where COVID-19 was identified as either the underlying cause of death or a contributing cause or condition that occurred from March 1 to July 31, 2020.
Dementia or Alzheimer's are the most common comorbidities associated with COVID-19 deaths
Of the over 9,500 COVID-involved deaths between March and July, the majority (90%) had at least one other cause, condition or complication reported on the certificate.
Dementia or Alzheimer’s were listed on the death certificate of 42% of the women and one-third of the men (33%) in COVID-involved deaths. (Chart 1). These results can be explained by the age profile of Canadians whose deaths involved COVID-19 over this period (54% were 85 years or older), as well as by their over-representation in long-term health care facilities. According to the Public Health Agency of Canada, about 1 in 4 Canadians aged 85 or older live with dementia or Alzheimer's.Note Moreover, more than half of seniors aged 80 or older who reside in long-term health care facilities live with dementia.Note During the first wave of the pandemic and up to the end of May, long-term care facilities and retirement homes accounted for more than 80% of all COVID-19 deaths in the country.Note

Data table for Chart 1
| Common COVID-19 comorbidities | Total | Male | Female |
|---|---|---|---|
| percent | |||
| Dementia or Alzheimer | 38 | 33 | 42 |
| Pneumonia | 33 | 36 | 31 |
| Hypertensive Disease | 15 | 14 | 16 |
| Ischemic Heart Disease | 13 | 16 | 11 |
| Respiratory Failure | 13 | 13 | 13 |
| Renal Failure | 12 | 13 | 11 |
| Diabetes | 12 | 14 | 11 |
| Symptoms and Signs NEC | 11 | 11 | 12 |
| Chronic Lower Respiratory Diseases | 10 | 10 | 10 |
| Nervous System Disorders excluding Alzheimer | 8 | 10 | 7 |
| Cancer | 8 | 9 | 7 |
|
Note: Comorbidities for deaths occurring between March 1, 2020 and July 31, 2020, where COVID-19 was involved. Source: Canadian Vital Statistics – Death Database (2020). |
|||
Other common comorbidities listed on COVID-involved death certificates included pneumonia (33%), hypertensive diseases (15%), ischemic heart disease (13%), respiratory failure (13%), renal failure (12%), diabetes (12%), symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (11%),Note chronic lower respiratory diseases (10%), nervous system disorders excluding Alzheimer's (8%) and cancer (8%). Many of these conditions are significantly more prevalent among Canadians aged 65 or older, who accounted for 94% of all COVID-involved deaths in the first wave. Chronic conditions are also more prevalent among lower income CanadiansNote , who may have been at increased risk of COVID-19 mortality during the first wave of the pandemic.
As a point of comparison, the most common influenza comorbidities recorded between 2016 and 2018 were similar to those recorded for COVID-19 during the first wave.Note
The prevalence of specific COVID-19 comorbidities varied with age
Dementia or Alzheimer’s were most often listed as comorbidities among Canadians aged 65 years or older whose deaths involved COVID-19—especially among those aged 85 or older (Chart 2).
Pneumonia, respiratory failure, symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified, and nervous system disorders excluding Alzheimer’s, such as Parkinsons’ or ALS were the most common comorbidities listed among COVID-involved deaths of Canadians aged 45 to 64 years old.
There were fewer than fifty COVID-involved deaths among those under the age of 45. Pneumonia, and symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified, were the most common comorbidities among this age group.
Healthy young adults, adolescents and children who contracted the virus have been the least likely to develop severe complications from COVID-19, including death. In fact, 100% of the COVID-involved deaths of Canadians under the age of 45 as of July 31 had at least one other disease or condition certified on the medical certificate of death. The proportion of those with at least one other disease or condition decreases with age, ranging from 93% for those aged 45 to 64 to 89% for those aged 85 years or older.
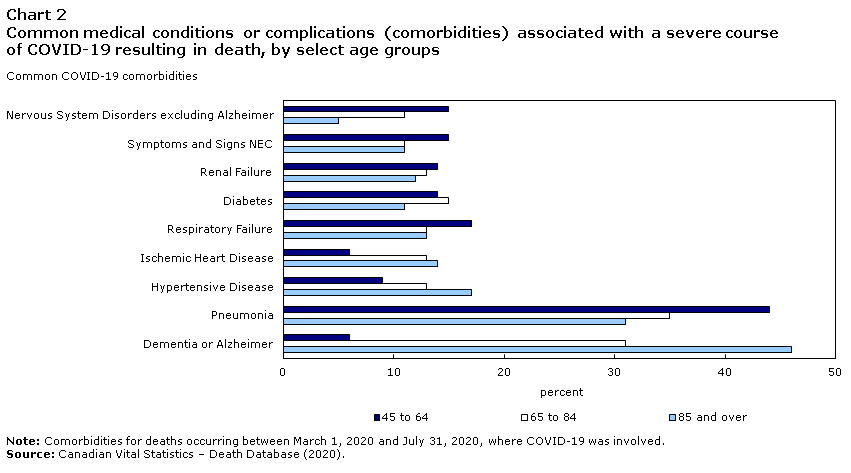
Data table for Chart 2
| Common COVID-19 comorbidities | 45 to 64 | 65 to 84 | 85 and over |
|---|---|---|---|
| percent | |||
| Dementia or Alzheimer | 6 | 31 | 46 |
| Pneumonia | 44 | 35 | 31 |
| Hypertensive Disease | 9 | 13 | 17 |
| Ischemic Heart Disease | 6 | 13 | 14 |
| Respiratory Failure | 17 | 13 | 13 |
| Diabetes | 14 | 15 | 11 |
| Renal Failure | 14 | 13 | 12 |
| Symptoms and Signs NEC | 15 | 11 | 11 |
| Nervous System Disorders excluding Alzheimer | 15 | 11 | 5 |
|
Note: Comorbidities for deaths occurring between March 1, 2020 and July 31, 2020, where COVID-19 was involved. Source: Canadian Vital Statistics – Death Database (2020). |
|||
The vast majority of COVID-19 deaths occurred in Quebec and Ontario
From March to July 2020, Quebec reported 6,240 COVID-involved deaths, more than double that reported in Ontario (2,770). Combined, these two provinces accounted for 95% of all COVID-involved deaths in Canada over this period.
As was the case nationally, dementia or Alzheimer’s were the most often cited medical conditions among COVID-involved deaths in Quebec (38%) and Ontario (36%) (Chart 3). However, renal failure was more frequently listed as a comorbidity in Quebec (13%) than in Ontario (10%), while diabetes was more often cited as a comorbidity in Ontario (14%) than in Quebec (11%).
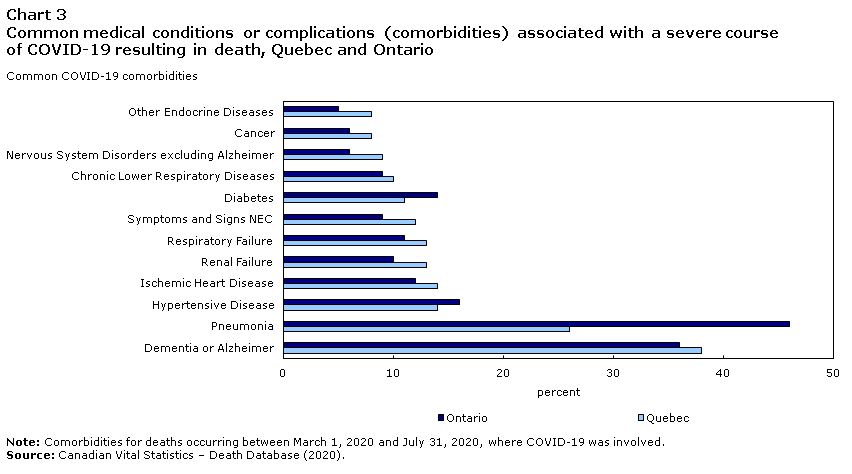
Data table for Chart 3
| Common COVID-19 comorbidities | Quebec | Ontario |
|---|---|---|
| percent | ||
| Dementia or Alzheimer | 38 | 36 |
| Pneumonia | 26 | 46 |
| Hypertensive Disease | 14 | 16 |
| Ischemic Heart Disease | 14 | 12 |
| Renal Failure | 13 | 10 |
| Respiratory Failure | 13 | 11 |
| Symptoms and Signs NEC | 12 | 9 |
| Diabetes | 11 | 14 |
| Chronic Lower Respiratory Diseases | 10 | 9 |
| Nervous System Disorders excluding Alzheimer | 9 | 6 |
| Cancer | 8 | 6 |
| Other Endocrine Diseases | 8 | 5 |
|
Note: Comorbidities for deaths occurring between March 1, 2020 and July 31, 2020, where COVID-19 was involved. Source: Canadian Vital Statistics – Death Database (2020). |
||
COVID-19 is also a contributing cause of death
Some deaths may have involved COVID-19 but were ultimately attributable to another disease such as ischemic heart disease, or an accidental injury such as a fall. These deaths do not consider COVID-19 as the underlying cause, but the virus was reported as being present on the medical certificate of death, either as a contributing cause or condition.
Nevertheless, COVID-19 was identified as the underlying cause of death in the vast majority (92%) of cases where COVID-19 was reported on the medical certificate (8,795 of the 9,525 deaths). In the other 8% of cases (730 deaths), cancer (170 deaths), dementia or Alzheimer’s (110 deaths), and other chronic conditions such as ischemic heart disease (105 deaths) or chronic lung disease (50 deaths) were most commonly found to be the underlying cause of death.
Conclusion
For the first time since the beginning of the pandemic in Canada, it is possible to estimate accurately the prevalence of comorbidities in COVID-19 deaths, as well as their prevalence by age. While that profile is still incomplete, future linkage of the CVSD to other data sources, such as the Canadian Census of Population, will highlight associations between COVID-19 and other factors. For example, the distribution of comorbidities may be studied by the socio-economic characteristics of the deceased, such as income, or by socio-cultural characteristics, such as membership to a specific population group designated as visible minorities. These and other topics will be the subject of complementary and upcoming analyses.Note
Data source
The authoritative source for cause of death data is the Canadian Vital Statistics Death Database (CVSD). Although not as timely as surveillance data, the CVSD does offer certain advantages in terms of understanding the direct and indirect effects of the pandemic. First, causes of death certified by medical professionals, coroners or medical examiners are recorded on the medical certificate of cause of death for all Canadians where the disease caused, or is assumed to have caused, or contributed, to death. As a result, the CVSD data will ultimately provide a more complete picture of the direct consequences of COVID-19.
Second, additional causes of death and conditions reported with COVID-19 can inform an examination of comorbid conditions or comorbidities.
In Canada, deaths are reported to Vital Statistics Offices as per provincial and territorial legislation. Deaths are registered by means of a standard death registration form which includes a medical certificate of cause of death section. The medical certificate of cause of death is completed by a physician, coroner or medical examiner or another qualified certifier with knowledge of the cause of death.
Provincial and territorial vital statistics agencies share information collected through the death registration process with Statistics Canada where it is compiled in the CVSD. In Canada, causes of death are coded to the 10th revision of the World Health Organisation's International Statistical Classification of Diseases and Related Health Problems (ICD-10).
Definition and certification of deaths due to COVID-19
For surveillance purposes, the WHO defines a death due to COVID-19 as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma). There should be no period of complete recovery from COVID-19 between illness and death.
In the international guidelines for certifying COVID-19 as a cause of death, certifiers are instructed to record COVID-19 on the medical certificate of cause of death for all decedents where the disease caused, or is assumed to have caused, or contributed to death. When certifying the cause of death, the physician, coroner or medical examiner is asked to report the sequence of morbid events leading to death as well as any conditions that contributed to that sequence. This is meant to reflect their informed opinion and can be reported with a single or multiple causes of death. When two or more causes are reported, the WHO ICD-10 rules and guidelines for coding and selecting the underlying cause of death for statistical tabulation are applied. The code for one cause is selected as underlying cause and the others are retained as multiple cause of death codes.
The COVID-19 death certification instructions include mention of the possibility that death may have been influenced by COVID-19 but caused by another disease or an unintentional injury.
In an effort to reach as many medical practitioners and other qualified certifiers as possible, Statistics Canada shared this information with federal, provincial and territorial partners
Selecting COVID-19 as Underlying Cause of Death
Deaths due to COVID-19, as displayed on Statistics Canada’s website, are those for which COVID-19 was found to be the underlying cause of death (UCOD), defined by the World Health Organization (WHO) as (a) the disease or injury which initiated the train of events leading directly to death, or (b) the circumstances of the accident or violence which produced the fatal injury.
When a pre-existing condition is suspected of putting a person at higher risk of a severe course of COVID-19 resulting in death, the death is counted as a death due to COVID-19 rather than a death due to the pre-existing condition.
It is also possible that the death may have been influenced by COVID-19 but caused by another disease or an unintentional injury event. In these situations, COVID-19 should still be recorded on the medical certificates of cause of death, but would not be considered a death due to COVID-19.
The statistics in this paper are based on deaths where COVID-19 was identified as the underlying cause of death in the provisional CVSD data, released on October 28th, 2020, and covering deaths occurring between January 1, 2020, and July 31, 2020.
Classification of deaths due to COVID-19
Statistics Canada and provincial and territorial vital statistics agencies use two codes to identify COVID-19 reported as a cause of death: U071 for COVID-19 specified as confirmed by a positive test result and U072 for COVID-19 described as “possible,” “probable,” or “pending a (positive) test result”. The total number of deaths due to COVID-19 is determined by adding counts in these two categories. The former also includes those deaths where the certificate makes no specification as “positive”, “possible,” “probable,” or “pending”. In Canada, the majority of COVID-19 deaths were classified as U071 (86%).
Another recommendation of the WHO is to capture mentions of negative COVID-19 test results using existing ICD-10 code Z038 (observation for other suspected diseases and conditions). Given the frequency certifiers reported COVID-19 negative on medical certificates of cause of death, Z038 is used by Statistics Canada and its partners. Currently, it tends to appear on records where a COVID death would be likely, such deaths attributed to pneumonia, dementia, or chronic lung disease.
- Date modified:
